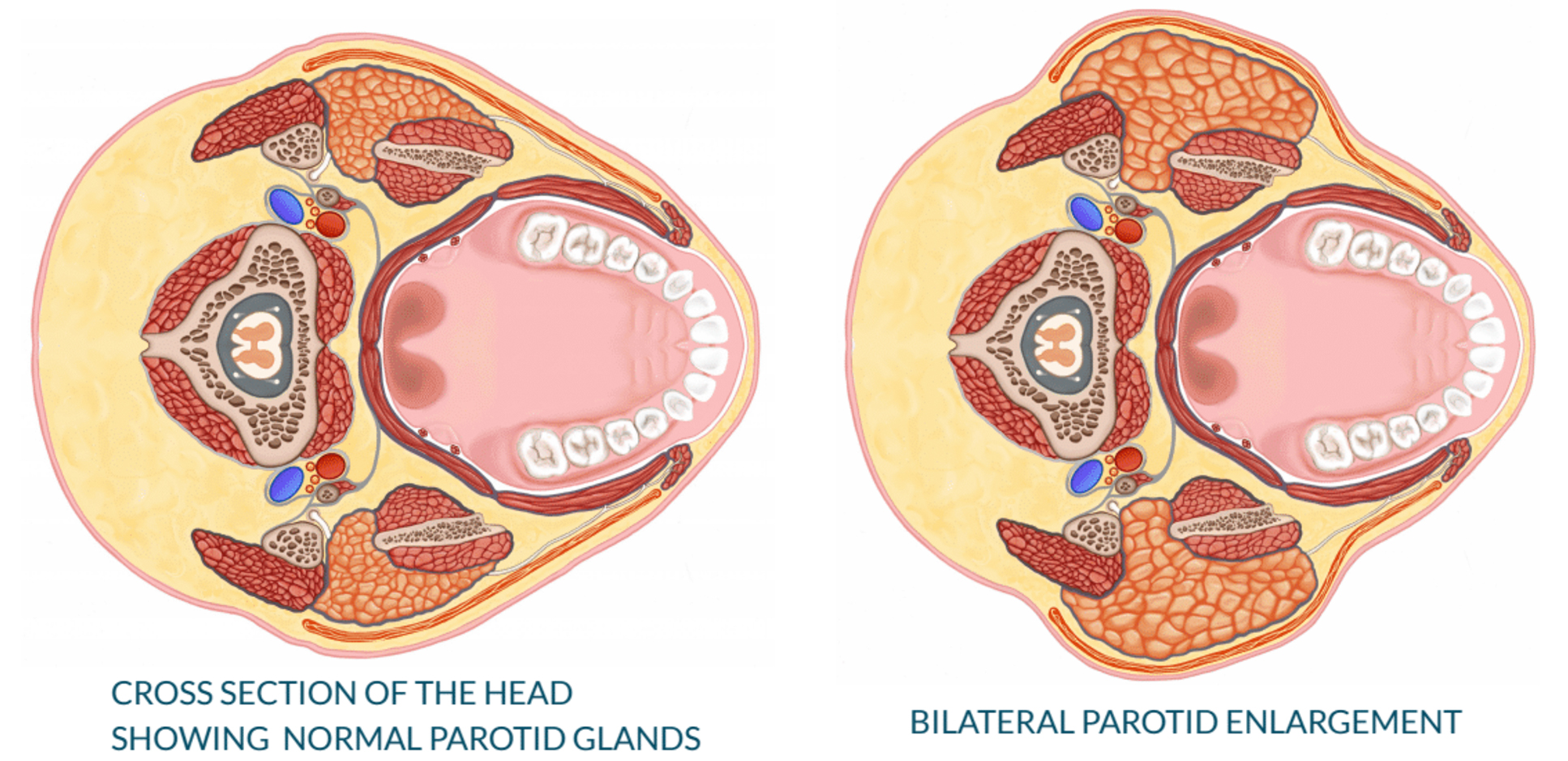
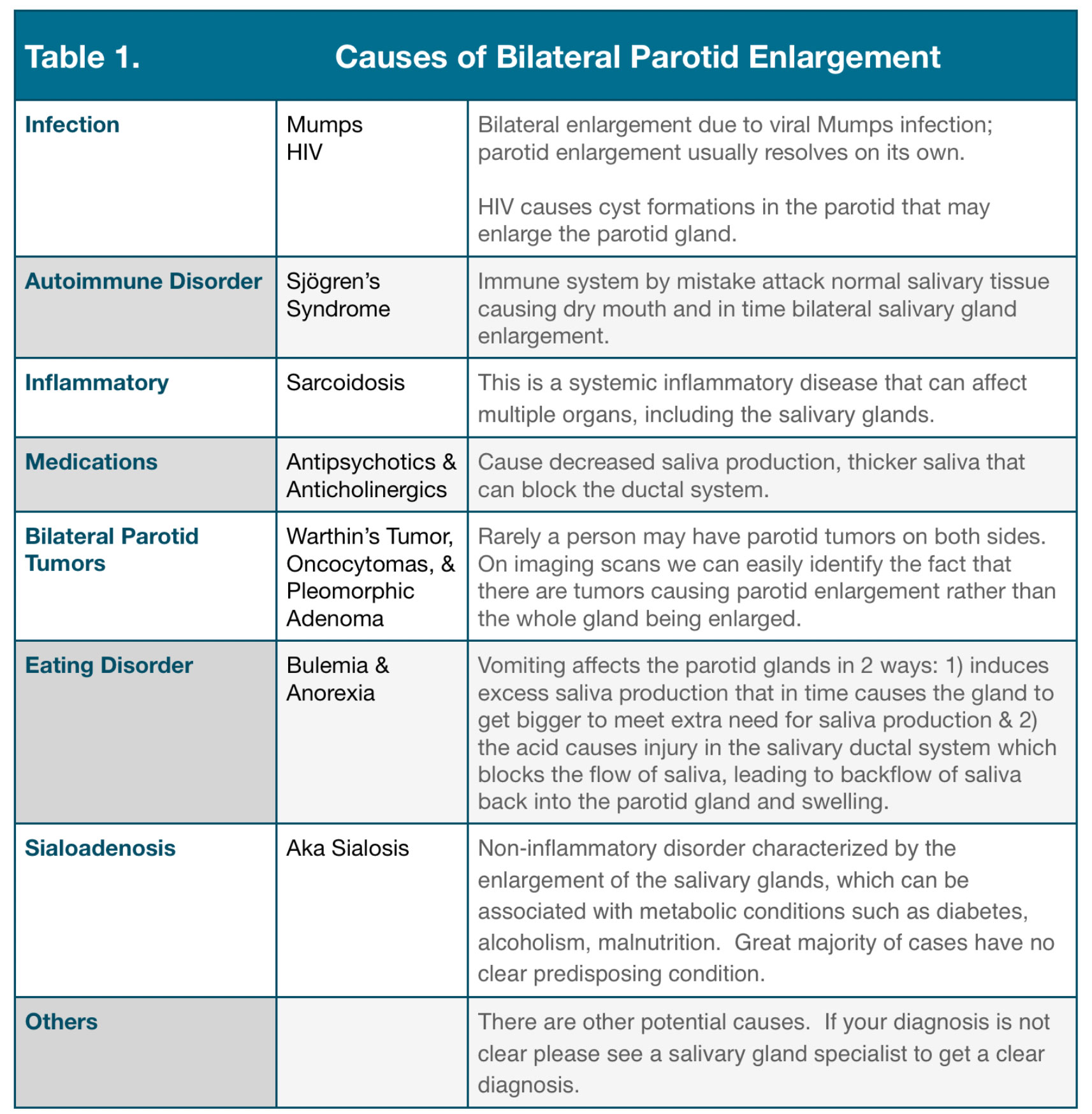
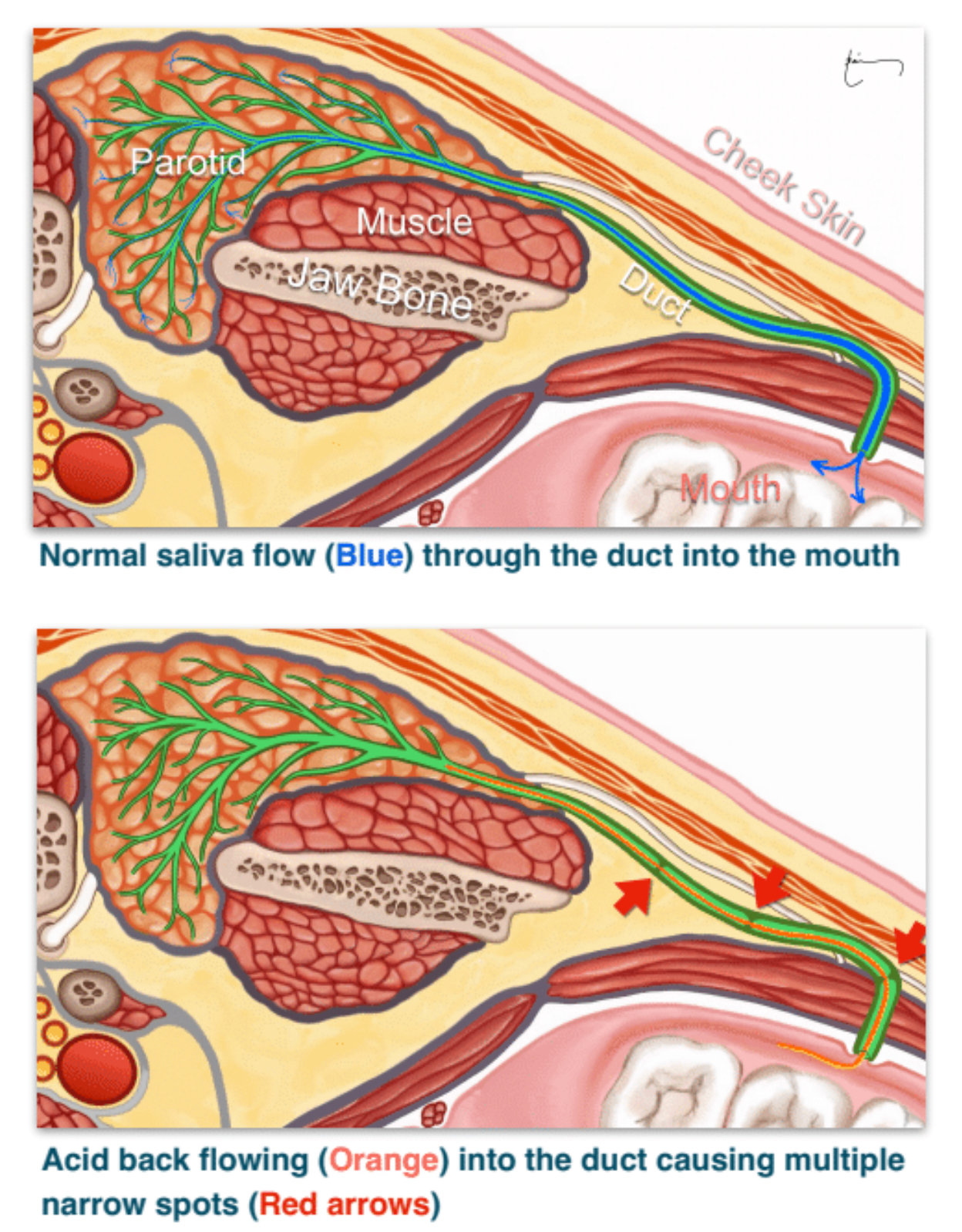
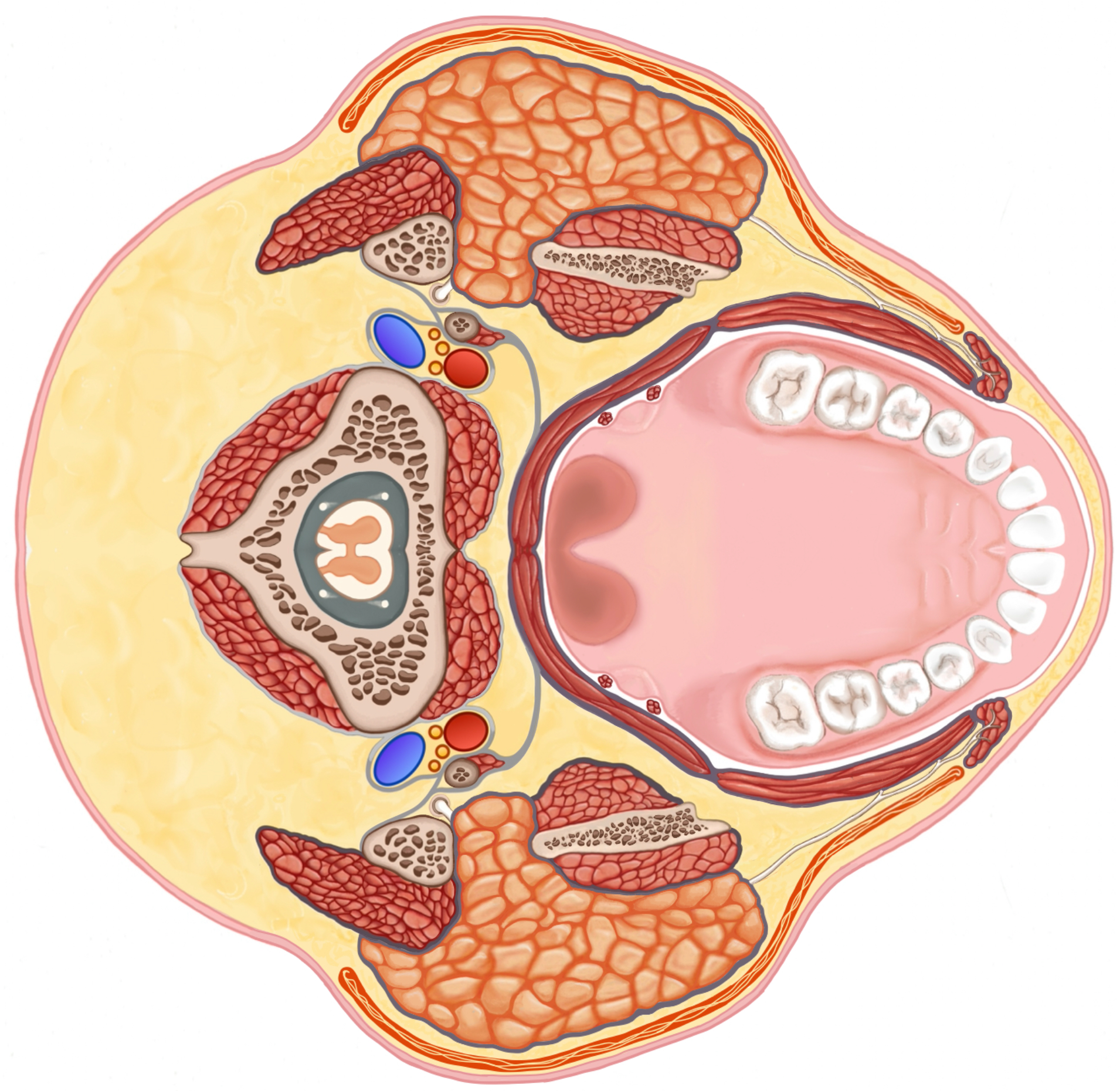
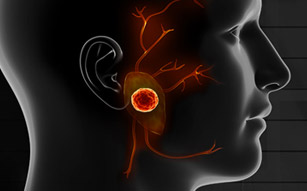
Sialosis – Also known as sialadenosis, is a non-inflammatory enlargement of the salivary glands. It is a chronic condition that is usually painless and bilateral. The most common salivary glands affected by sialosis are the parotid glands, however, the submandibular & sublingual glands can also be affected.
The exact cause of sialosis is unknown, but it is thought to be due to a combination of factors, including:
Abnormal nerve function: The salivary glands are innervated by the autonomic nervous system. It is thought that sialosis may be caused by abnormal nerve function that stimulates the salivary glands to become overactive and grow.
Hormonal imbalances: Sialosis has been associated with hormonal imbalances, such as hypothyroidism and diabetes.
Medications: Some medications, such as lithium and diuretics, have been linked to sialosis.
Alcoholism: Alcoholism is a common cause of sialosis.
Nutritional deficiencies: Malnutrition, particularly vitamin A deficiency, has been linked to sialosis.
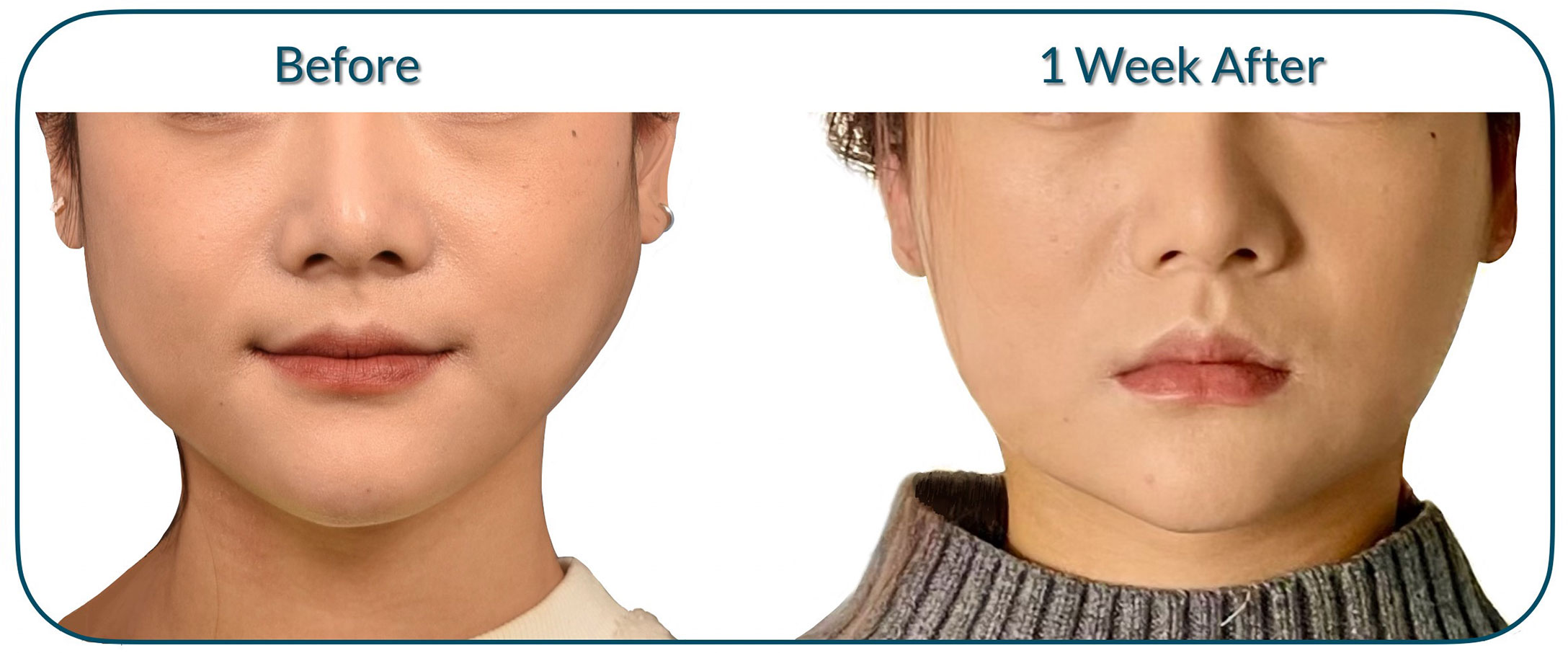
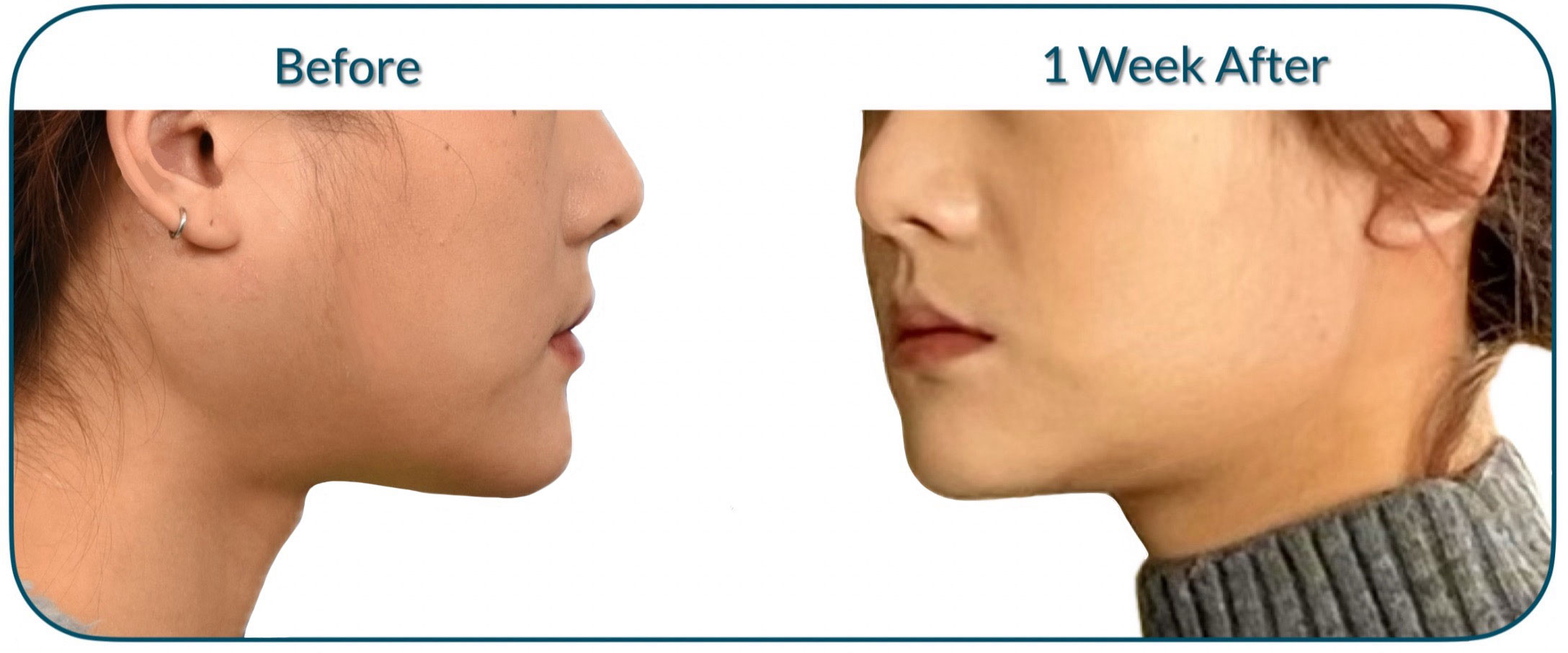
The symptoms of sialosis can vary depending on the severity of the condition. Some people may experience only mild swelling of the salivary glands, while others may experience more severe swelling, pain, and difficulty opening the mouth.
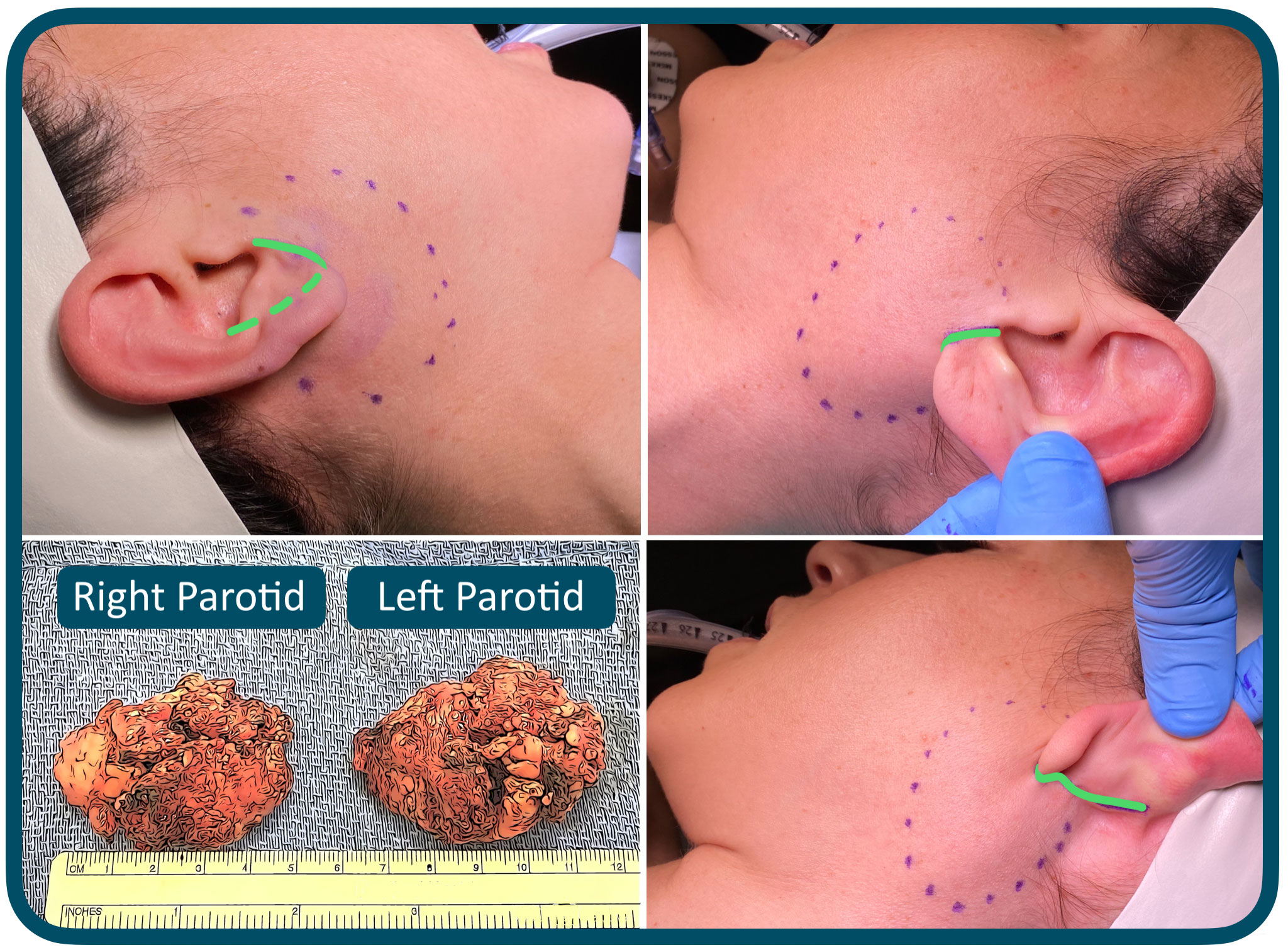
The diagnosis of sialosis is usually made based on the patient’s medical history and physical examination. Imaging tests, such as ultrasound or MRI scan, may be used to confirm the diagnosis and rule out other conditions. In some cases, a biopsy may be performed to rule out other possible causes of glandular enlargement.
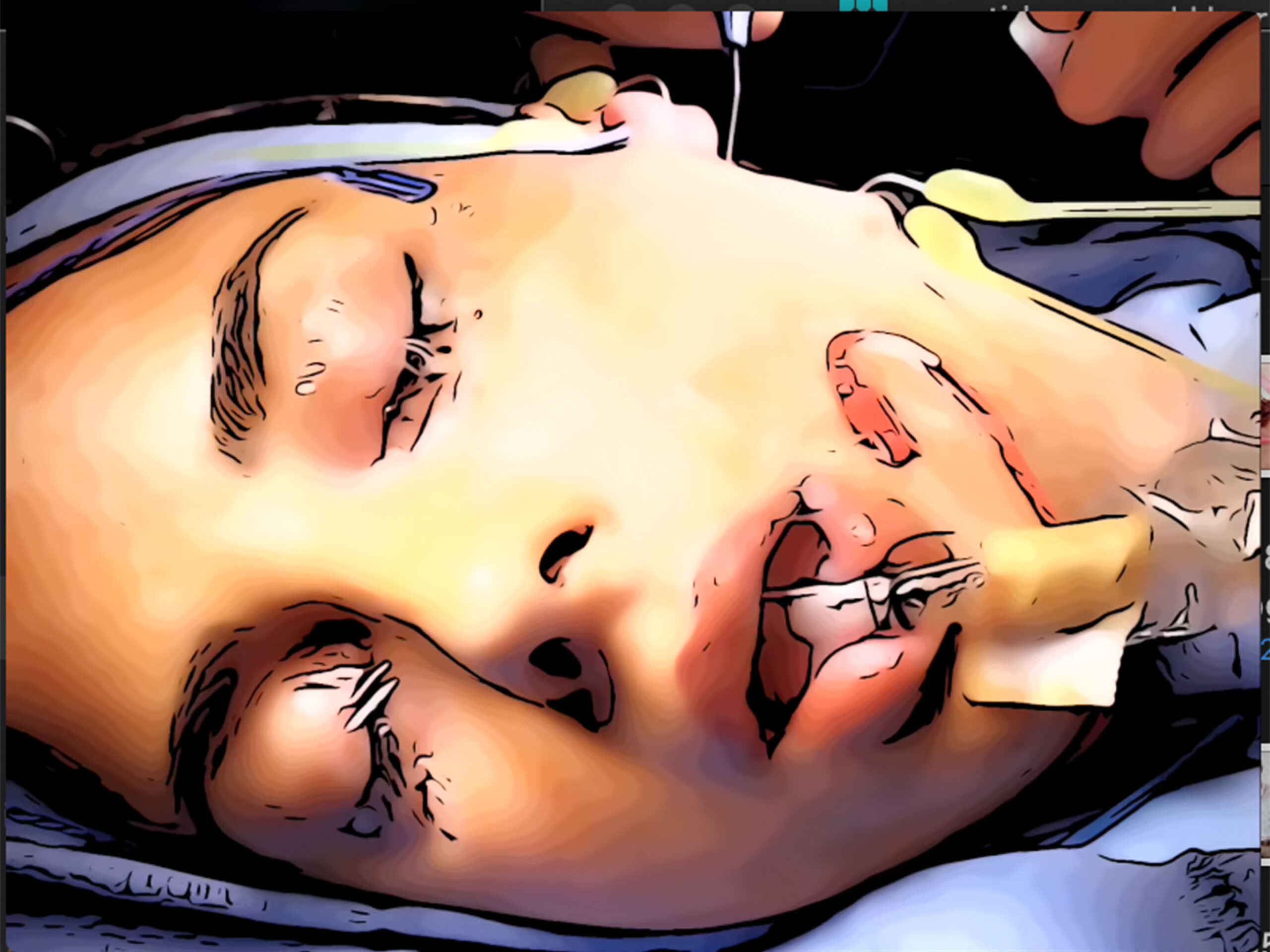
The treatment of sialosis aims to alleviate symptoms and manage any underlying conditions contributing to the disorder. This may involve addressing metabolic disorders, adjusting medications, or providing supportive care for dry mouth symptoms. Saliva substitutes and good oral hygiene practices can help manage the dry mouth symptoms and reduce the risk of dental complications. In severe cases, surgical intervention may be necessary to remove the affected salivary glands.