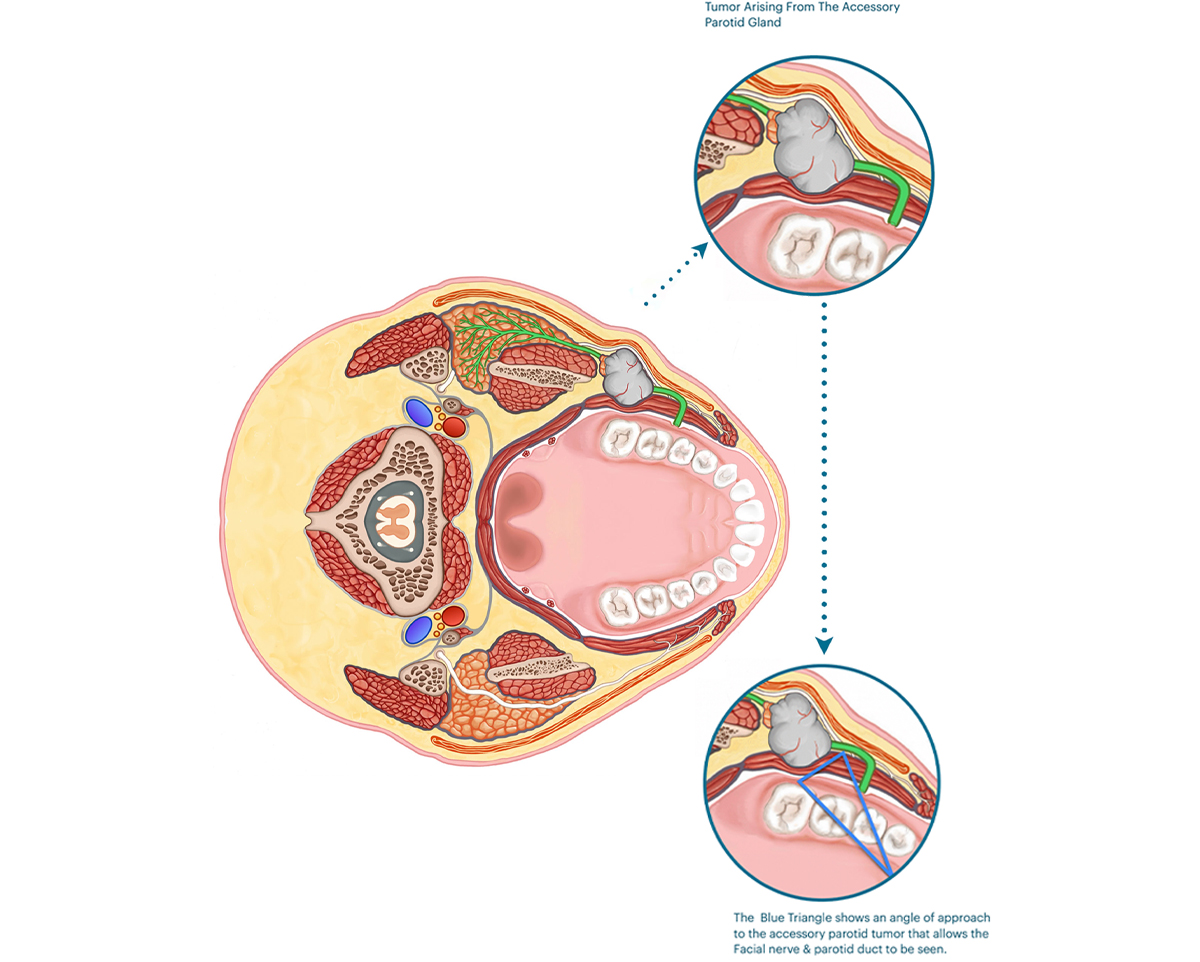
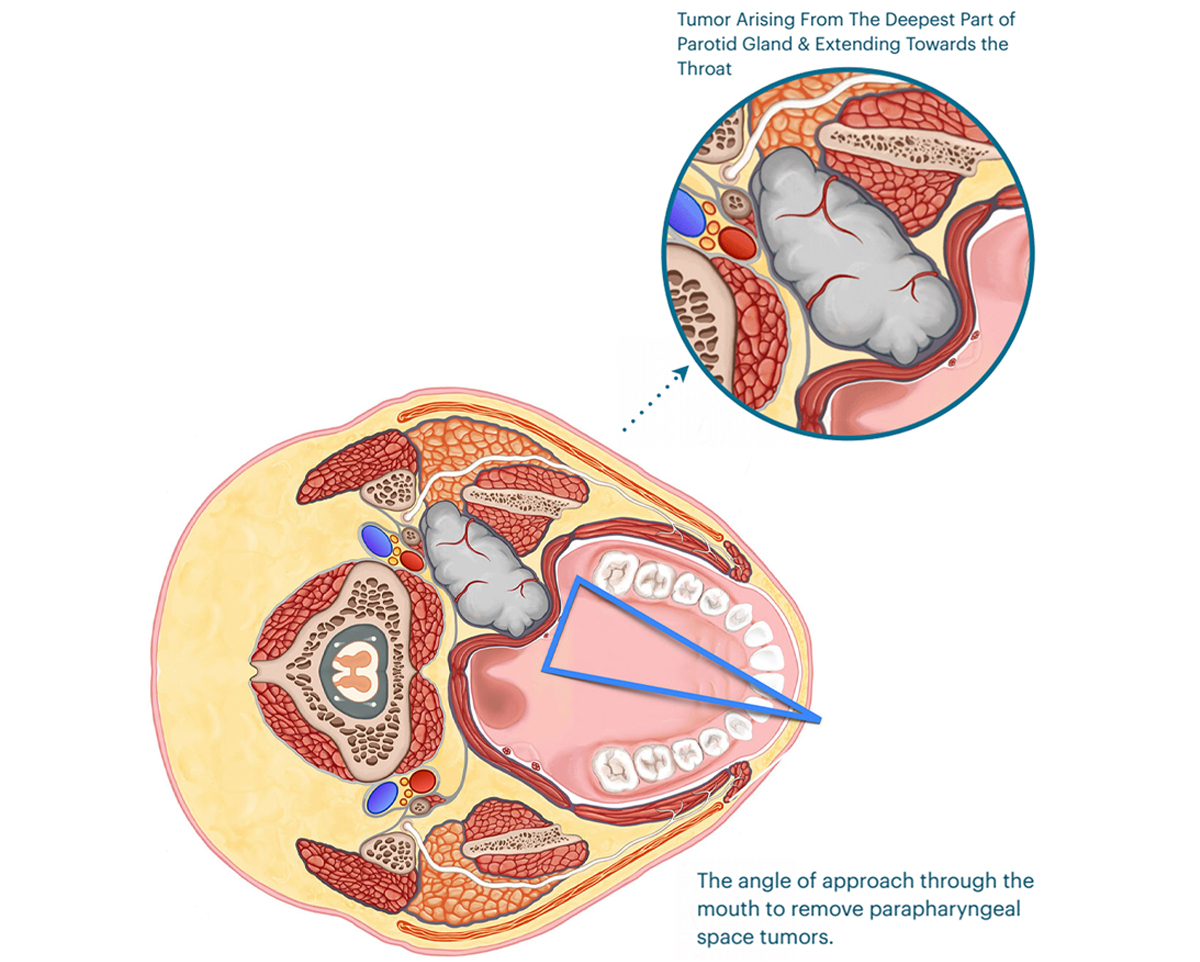
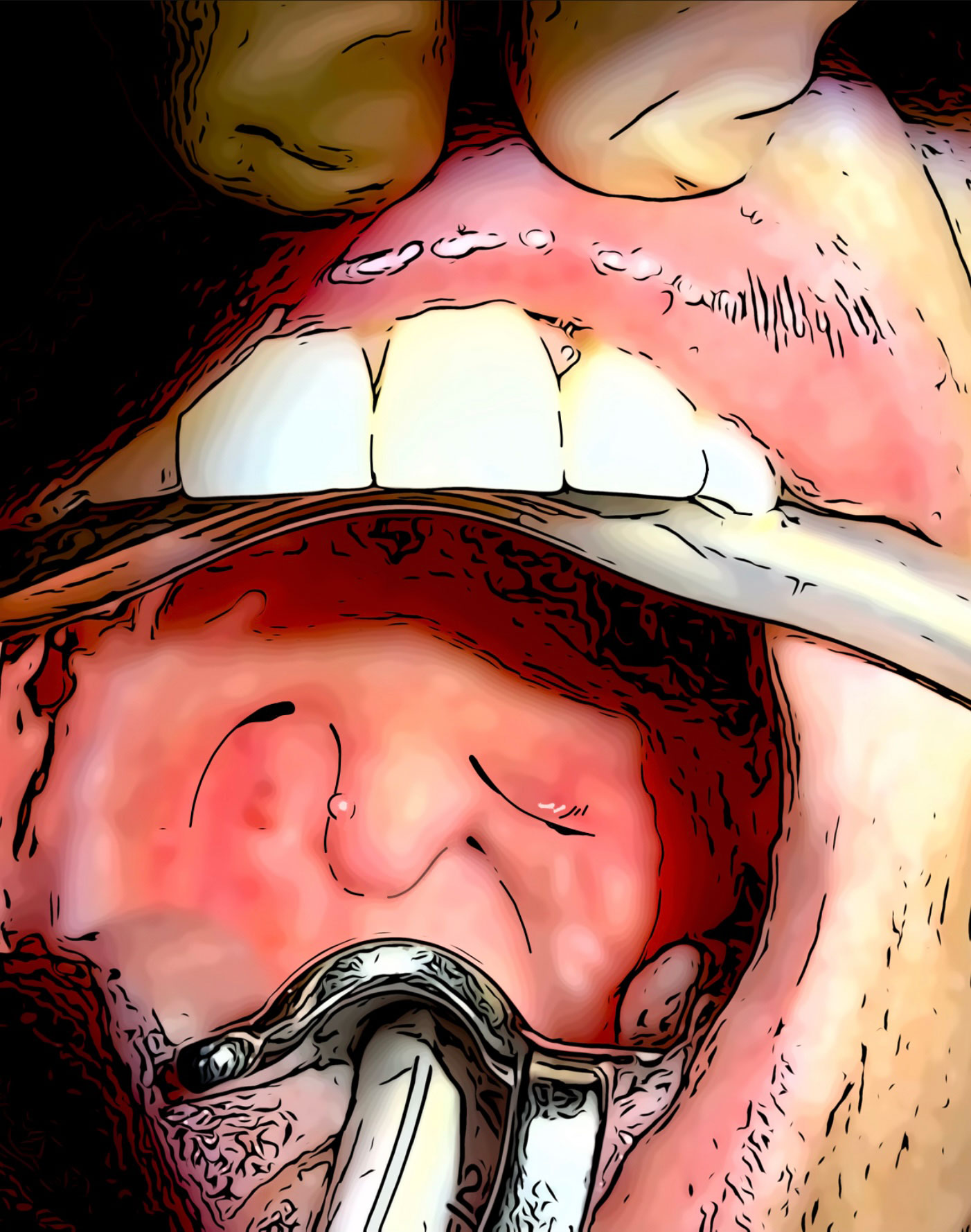
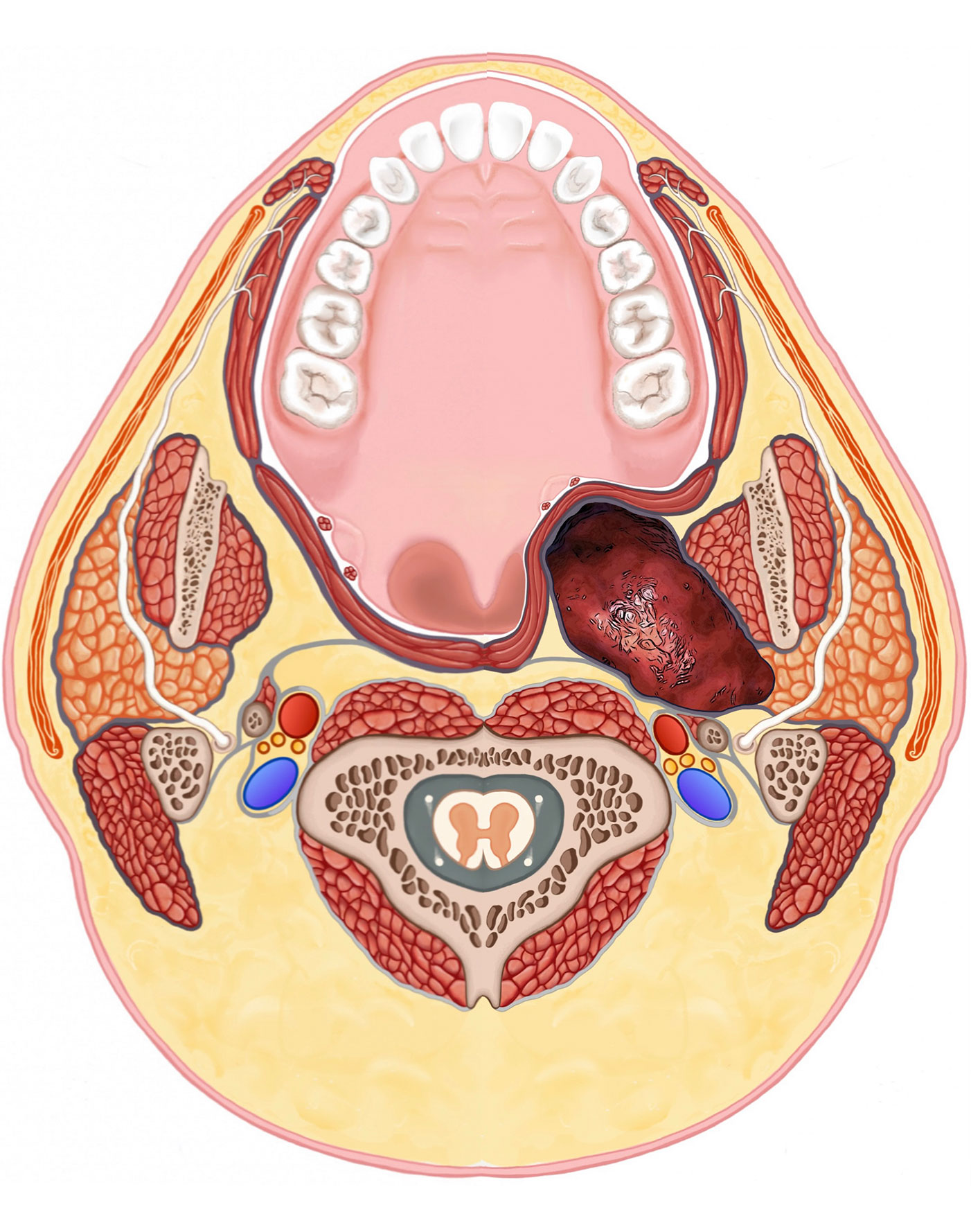
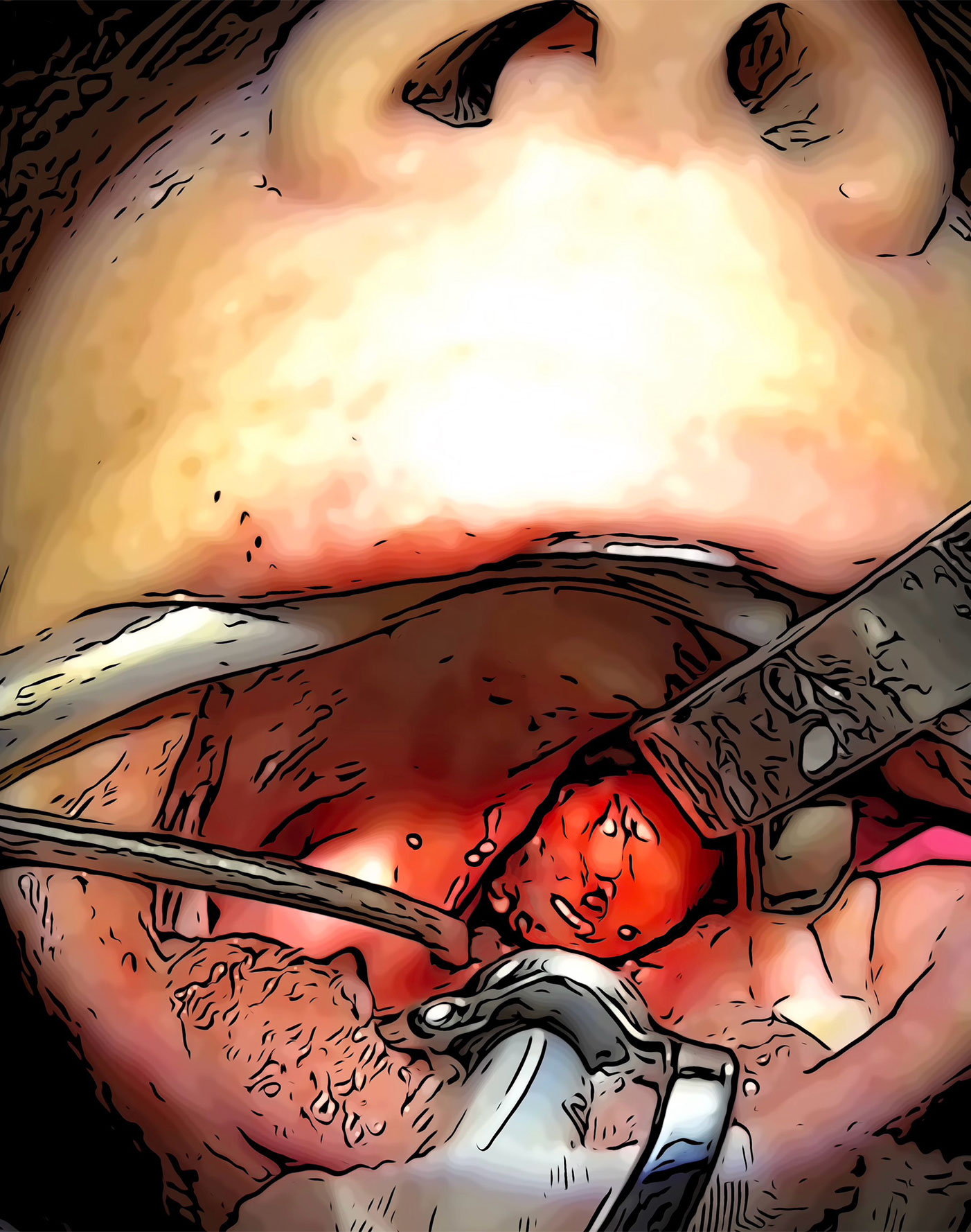
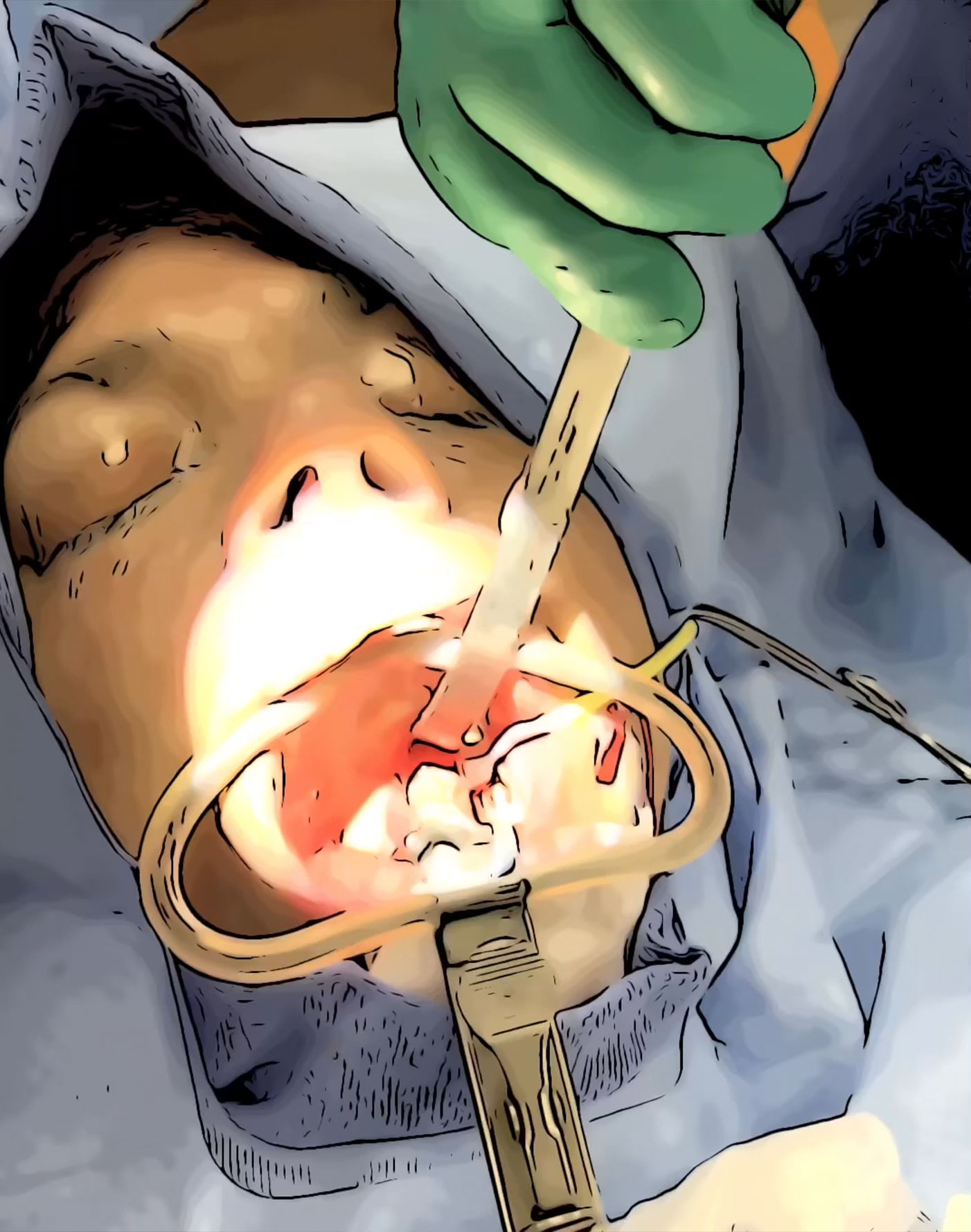
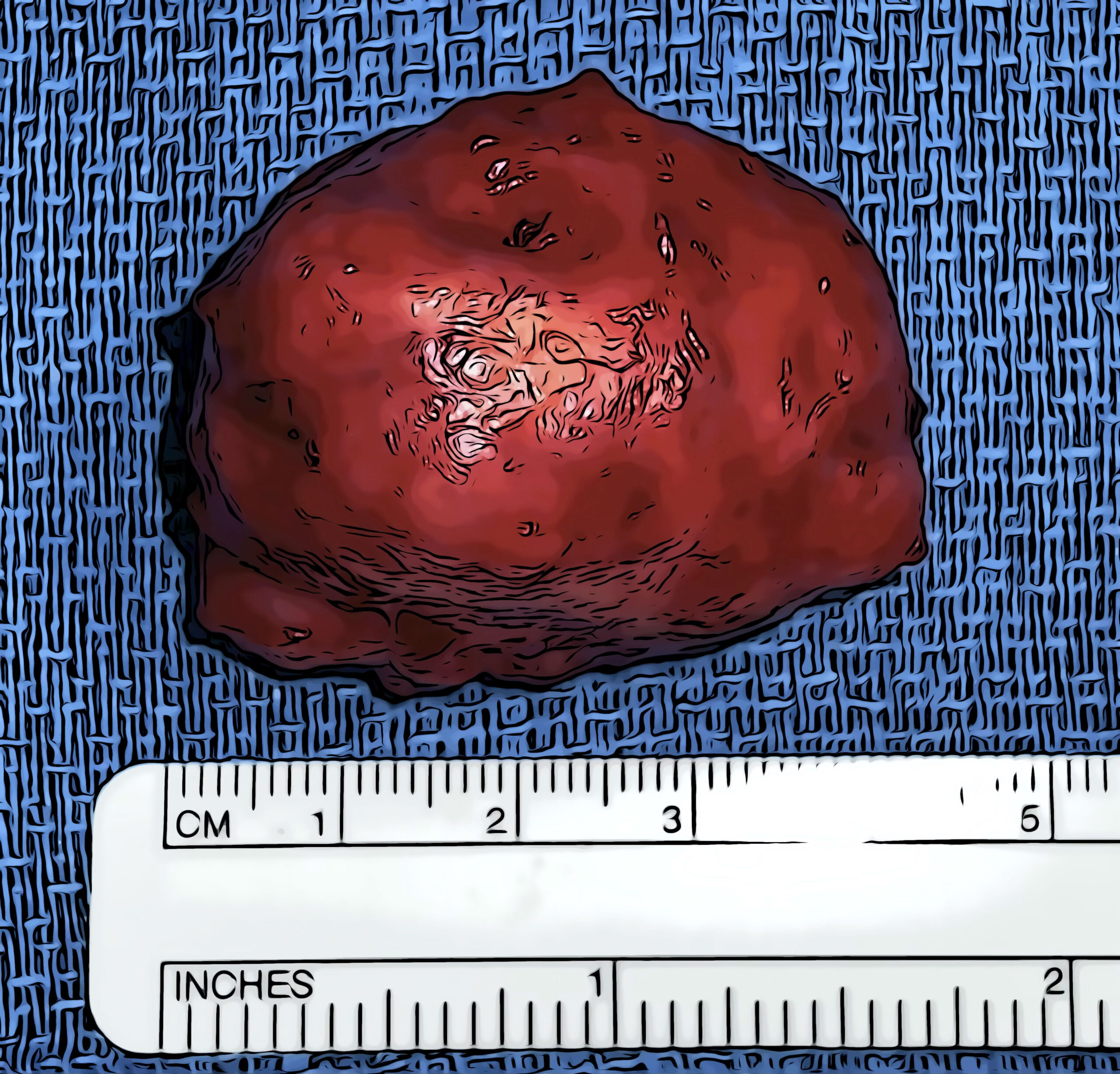
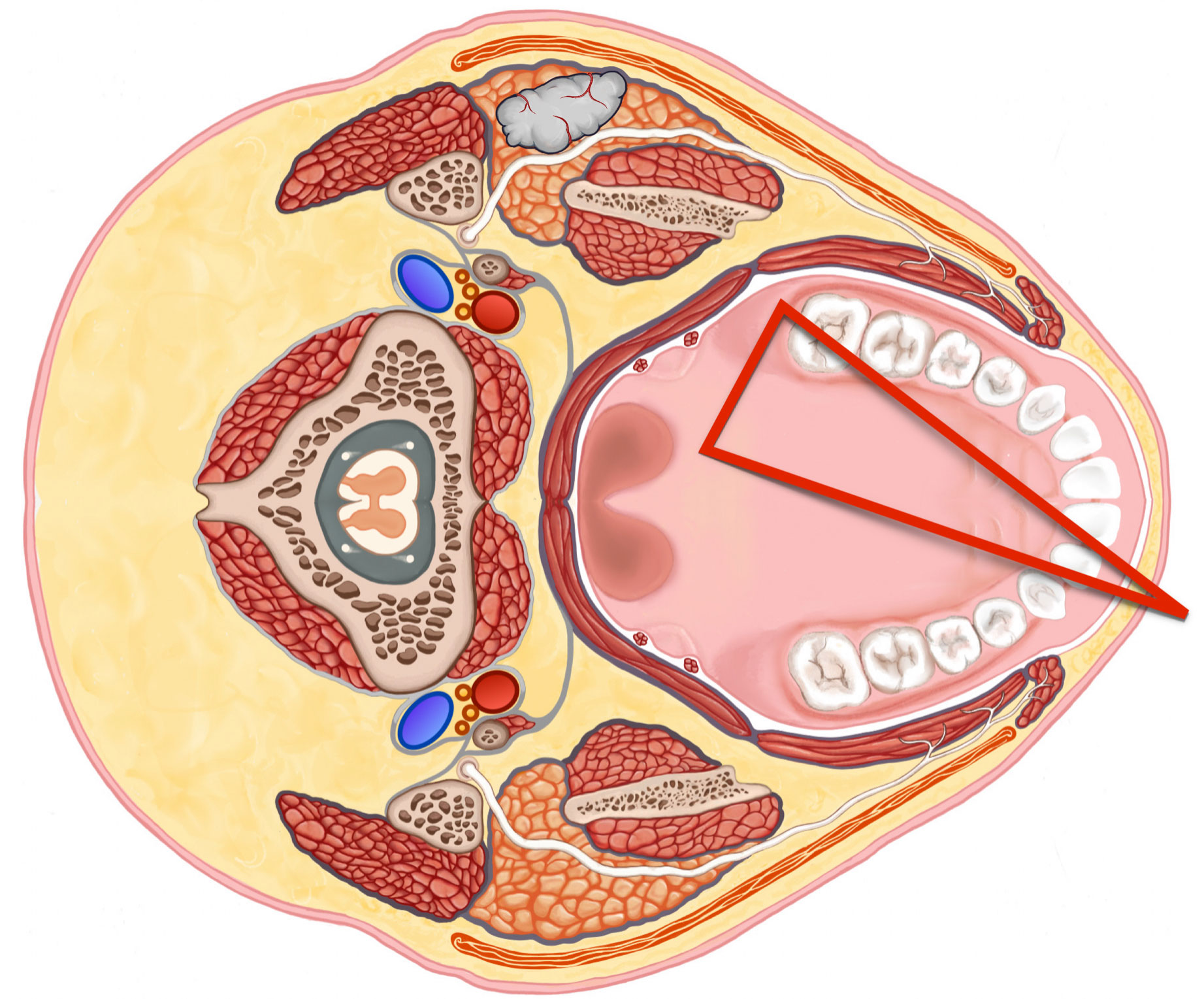
There are 2 anatomical locations of parotid tumors that allow safe removal through mouth. In this section we’ll discuss the locations and how the surgery is done. The two locations are (1) tumors that are in the accessory parotid glands, and (2) parapharyngeal space tumors. Both of which can either be seen through the mouth or felt on examination.
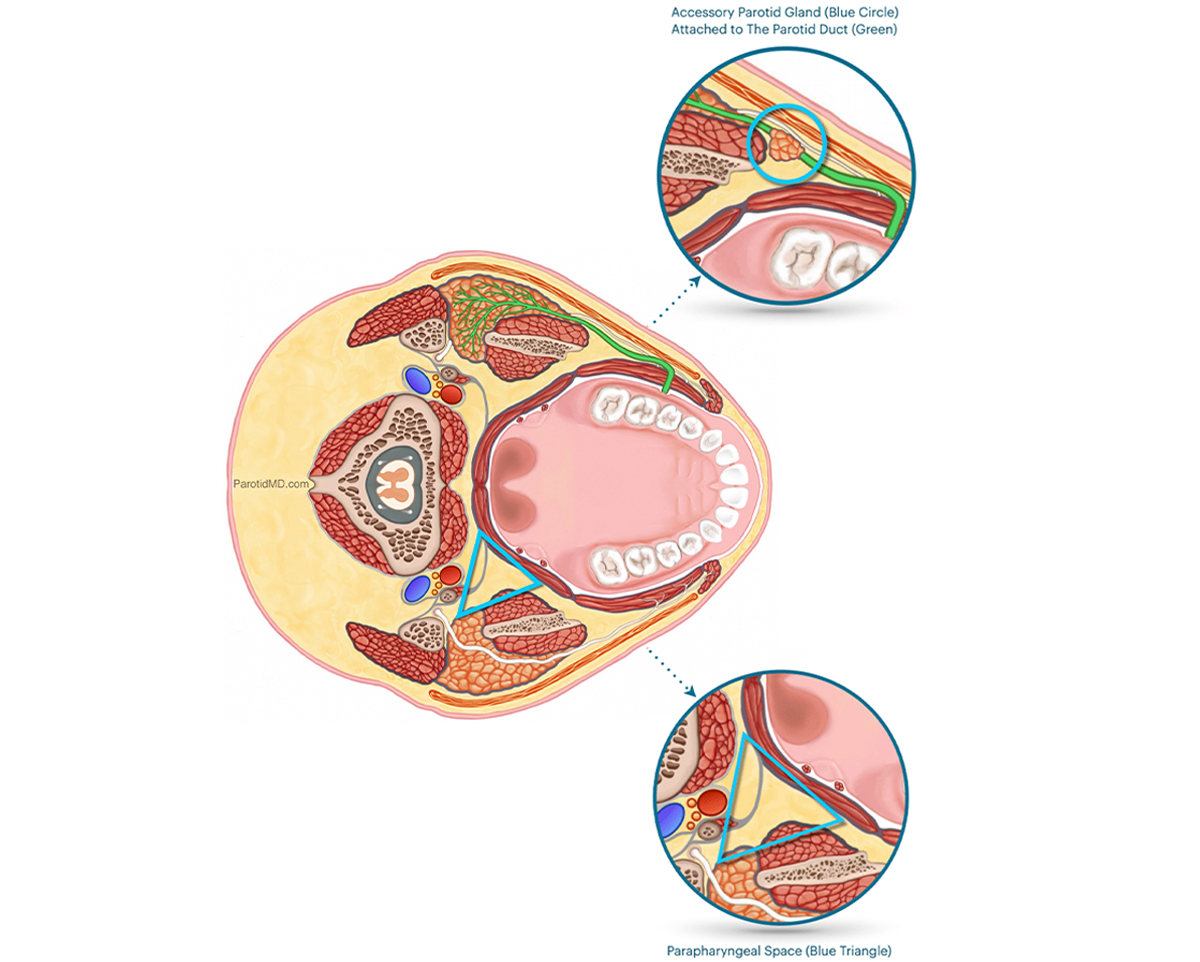
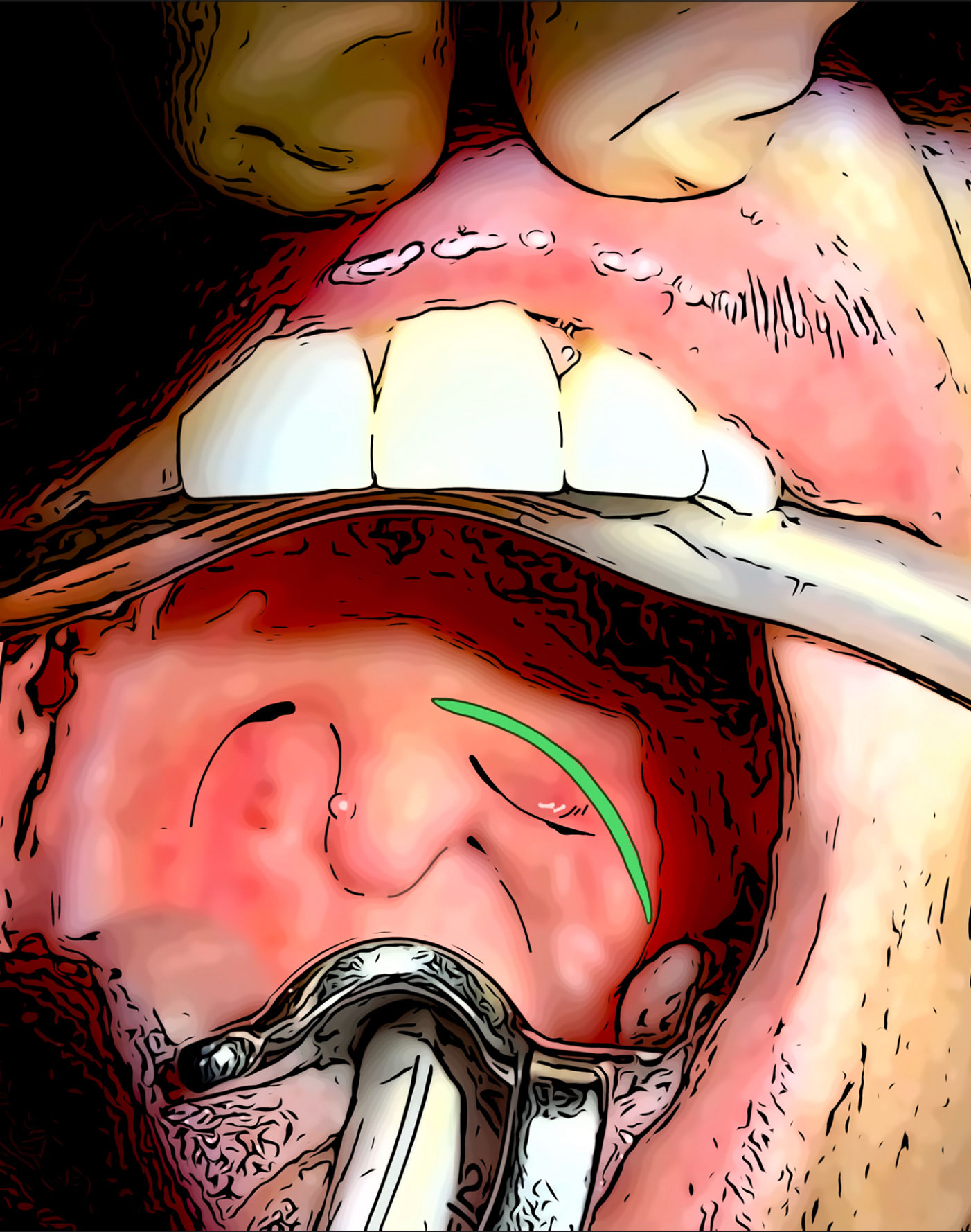
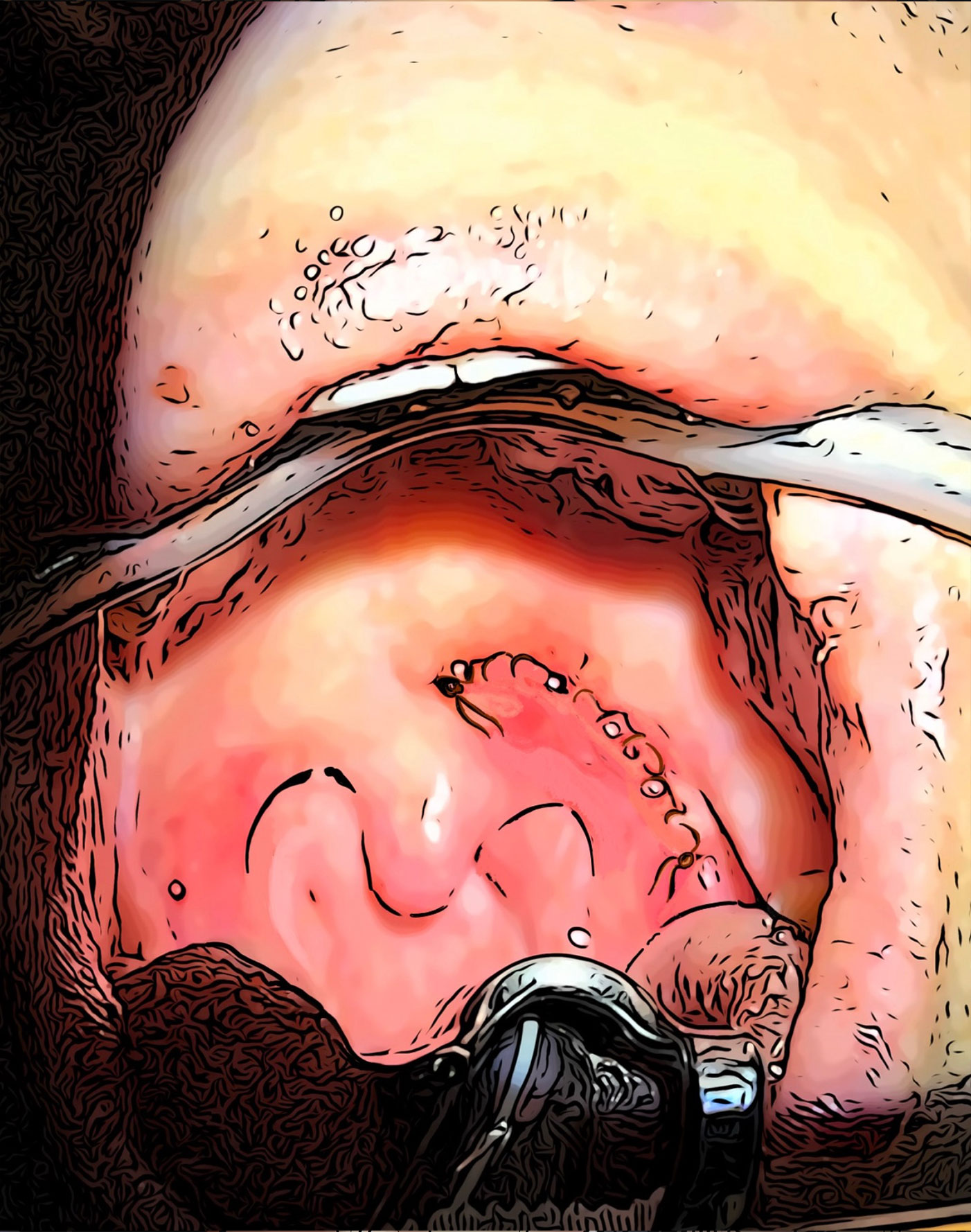
The accessory parotid gland is a portion of the parotid gland that gets dragged forward by the duct (green) the develops in the gland & travels forward towards the mouth in the developing fetus. The accessory parotid glands are deep to the facial nerve and closer to the mucous membrane on the inside of the cheeks.