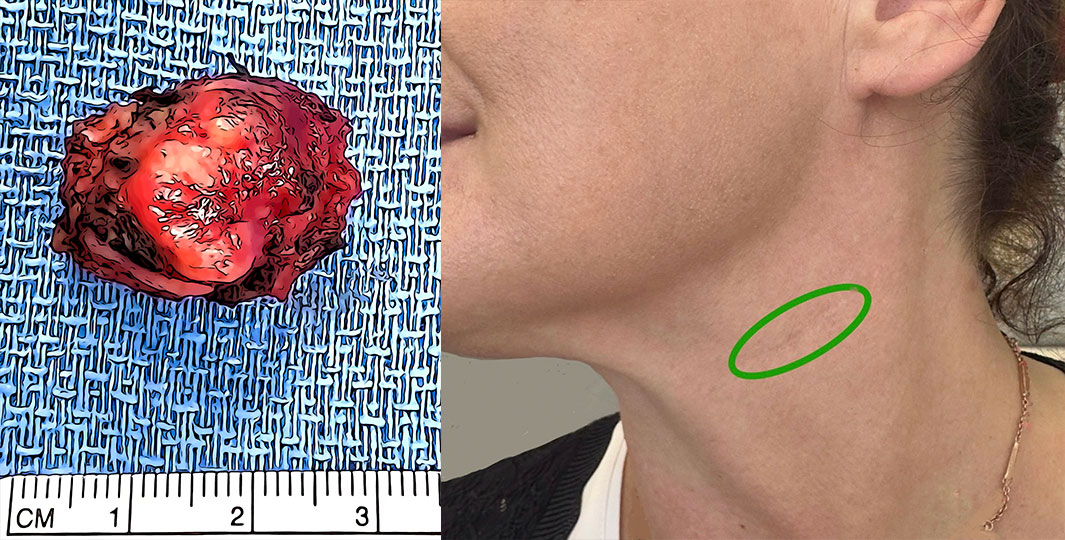
What happens if a parotid cancer is not treated?
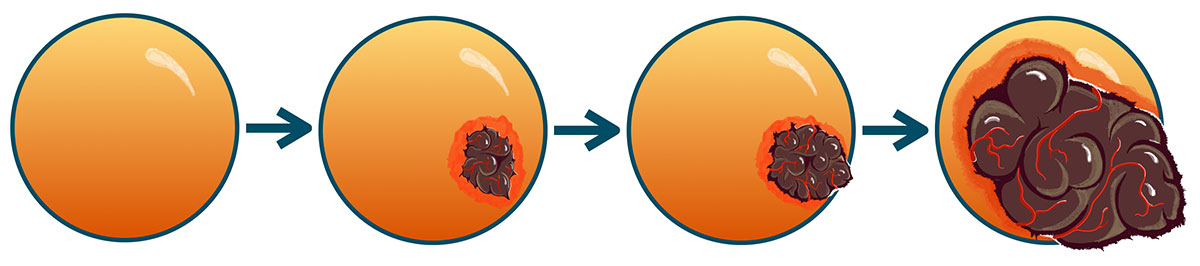
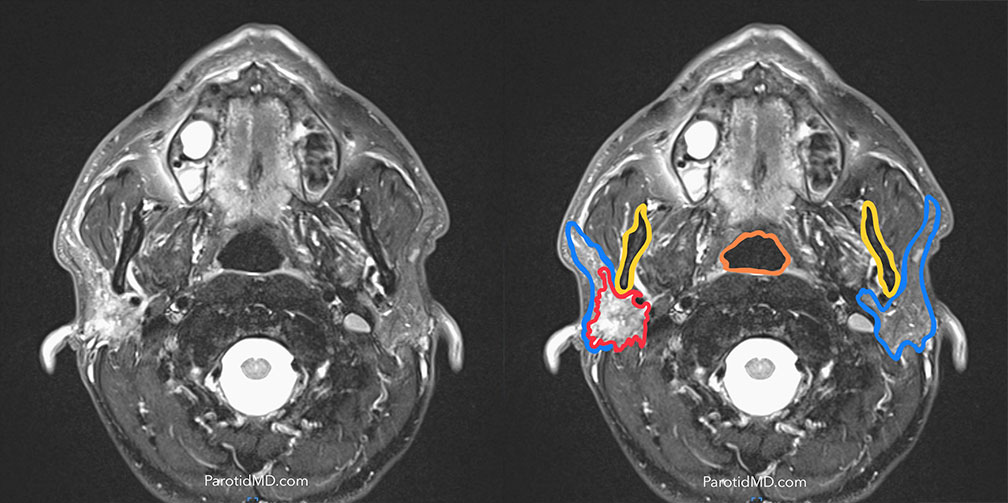
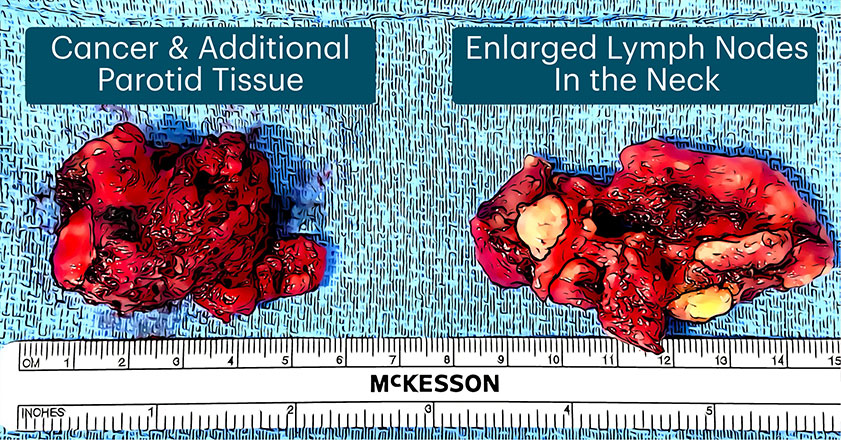
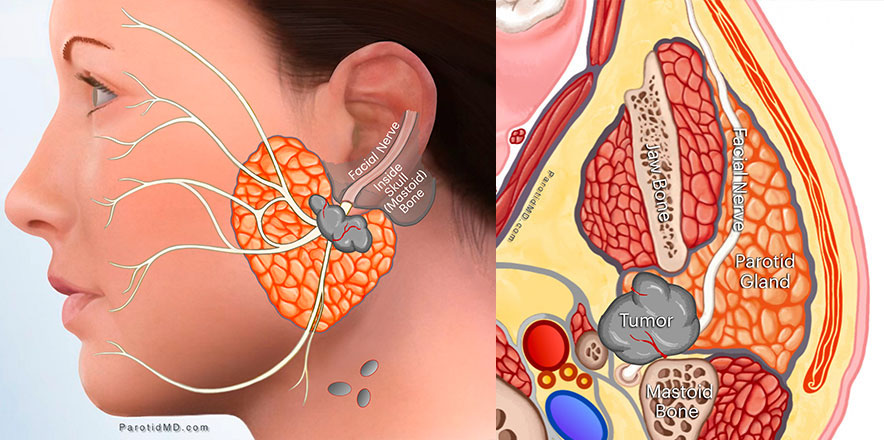
The cancer continues to grow. As it grows more mutations (genetic mistakes) occur that take away inhibitions (or control commands). In time the cancer will invade the facial nerve and cause the nerve to stop working which will lead to facial paralysis. As it continues to grow more changes occur (mutations in control commands) in the cancer that allows it to exist outside of the parotid gland. Once this occurs the cancer can travel through lymph or blood vessels and spread to other parts of the neck or the whole body. Generally speaking, as parotid cancer grow they cause the problems (complications) a person would be afraid of with surgery.
Can parotid tumors be treated with natural remedies with success?
I wish that would be the case. Because all cancers arise from mutations in the genetic code, and those mutations/ mistakes are passed along to all the children of the cancer cells, a natural treatment that could eradicate the disease has to correct all the mutations in all of the cancer cells. When a cancer is 2mm wide it will contain 1 million cells. So the treatment would have to correct the genetic mistakes in millions of cells at the same time.
The alternative is to use supplements to boost the immune system, however since these millions of cancer cells have already evaded the immune system, it is unlikely that immune boosters alone would be able to eradicate the cancer. There are natural remedies, that in my experience, can help the our bodies with the fight against cancer, however, they should be used in conjunction with know effective treatments rather then instead.
Can a salivary cancer be treated without surgery?
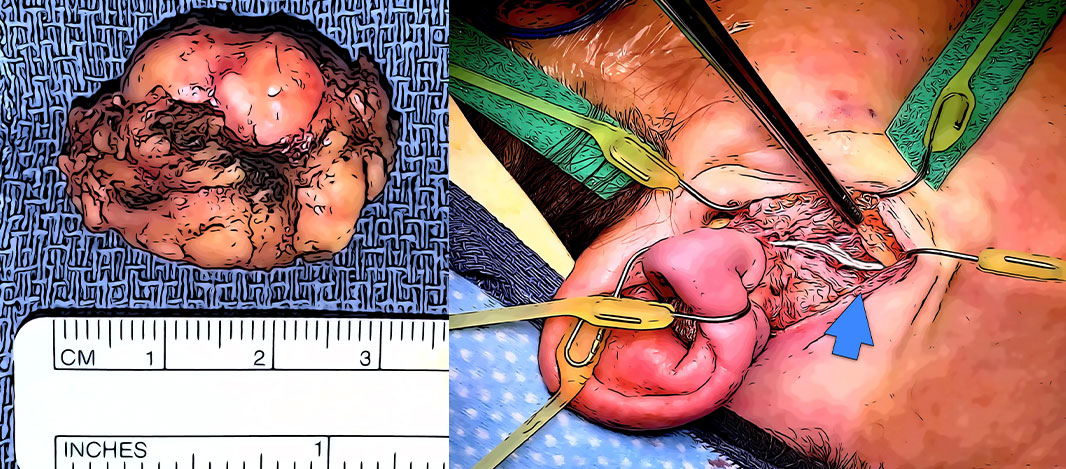
The primary treatment for salivary gland cancers is surgery. Non-surgical treatments such as chemotherapy combined with radiation therapy have a much much lower chance of cure, and are generally reserved for those who are either too ill to undergo surgery, or their cancer is so advanced that surgery would not be able to get around the cancer and remove it.
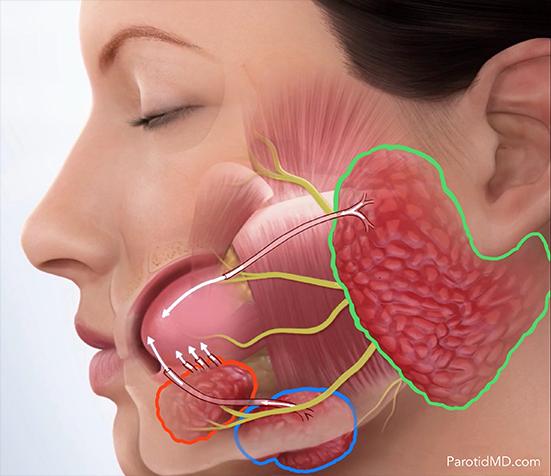
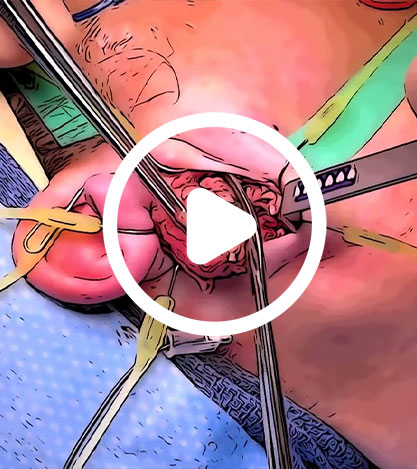
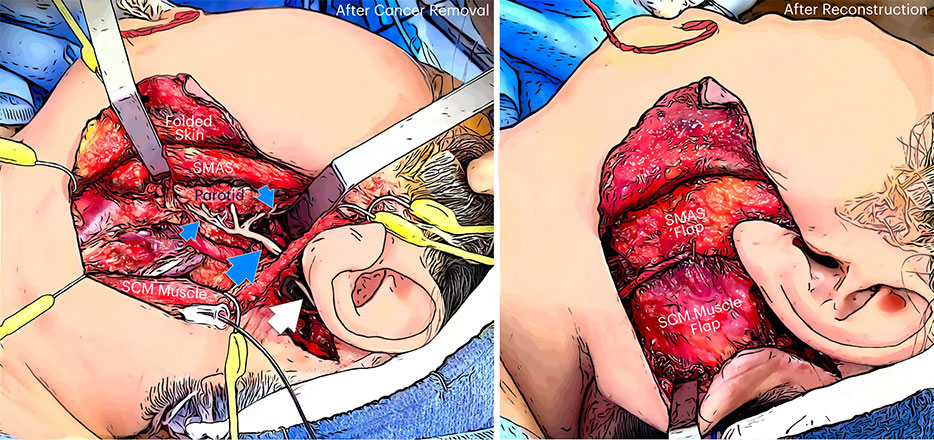
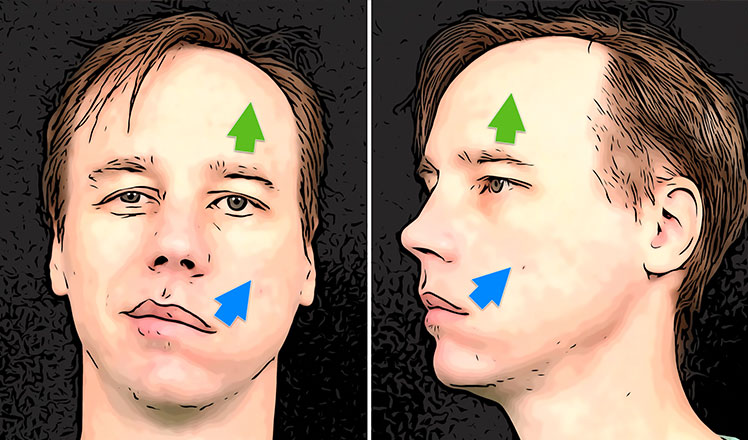
Is the facial nerve cut with every cancer parotid surgery?
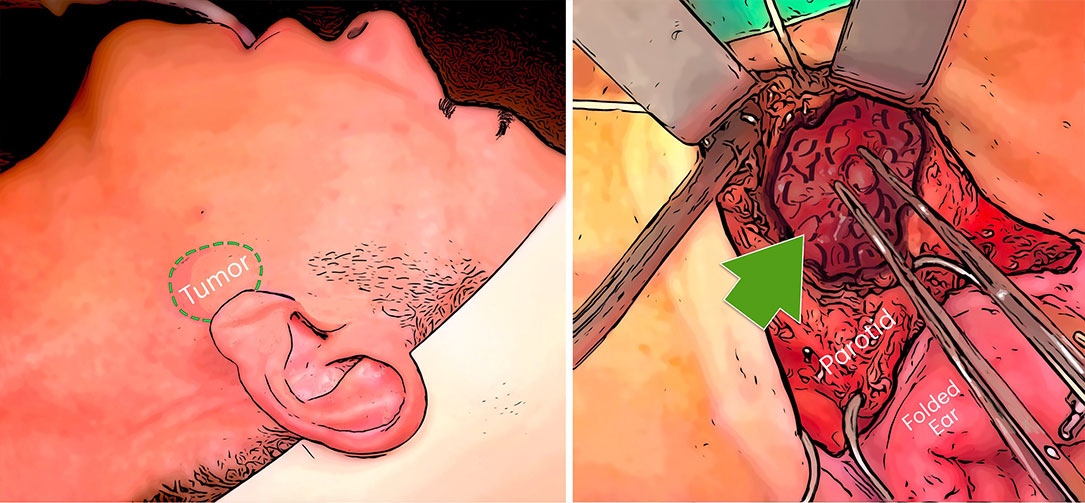
Absolutely not. If the facial nerve is fully functional before surgery, then every effort must be made to save the facial nerve and all its branches. This will require experience, dedication, and immense patience. At the CENTER we firmly believe this is time well spent and worth spending to save the facial nerve. The facial nerve and facial movements are exceeding important, and I would say much more important than one would imagine.
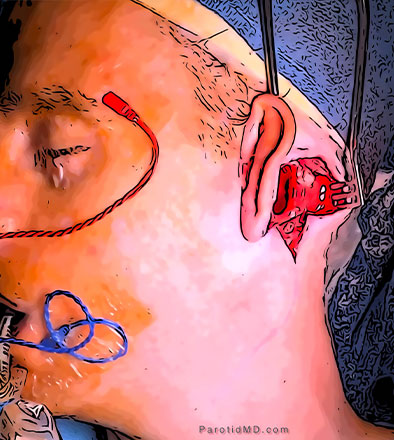
Most of the time when the facial nerve is involved with cancer, there are signs. At first, the facial muscles may start to twitch and then become weak before becoming fully paralyzed. There are the very rare cases, where during the surgery we find the nerve is wrapped by the cancer without any symptoms.
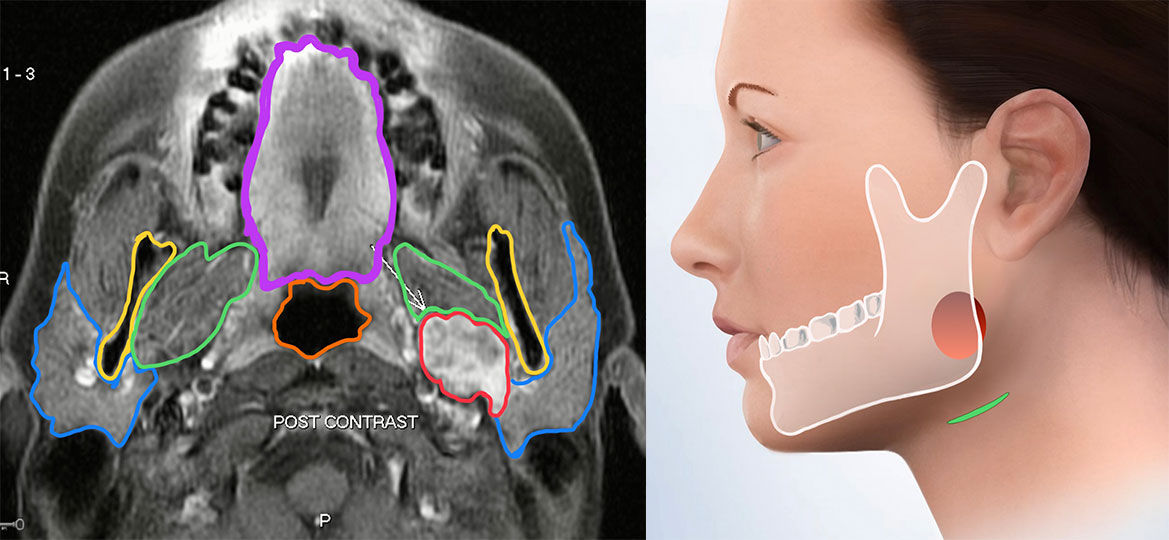
Are there any scans that would tell us the facial nerve is involved when it is fully functional?
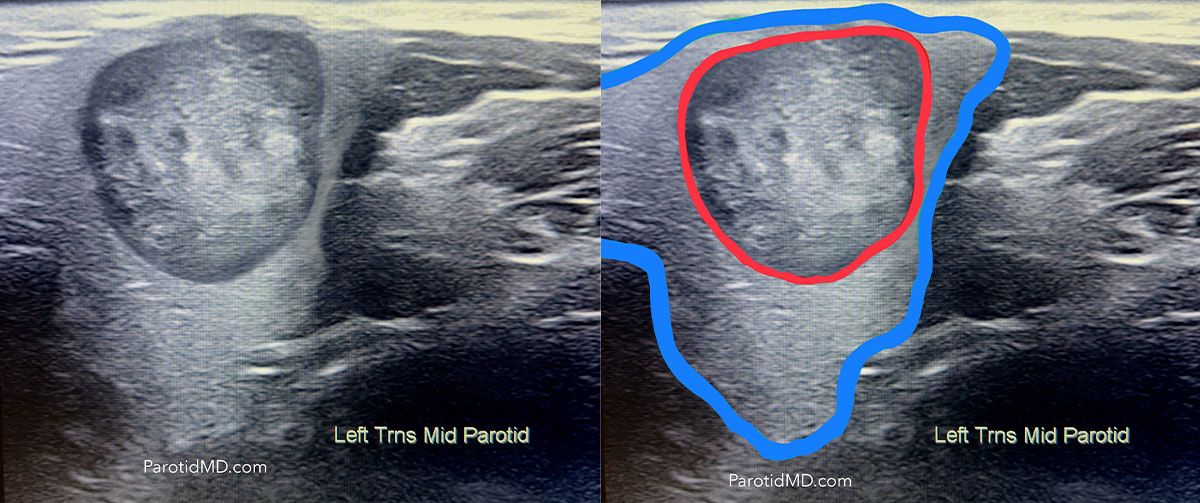
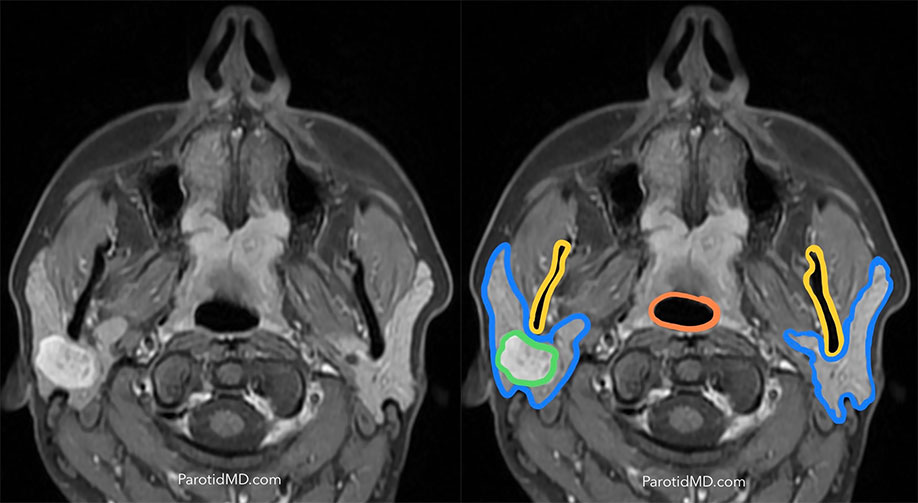
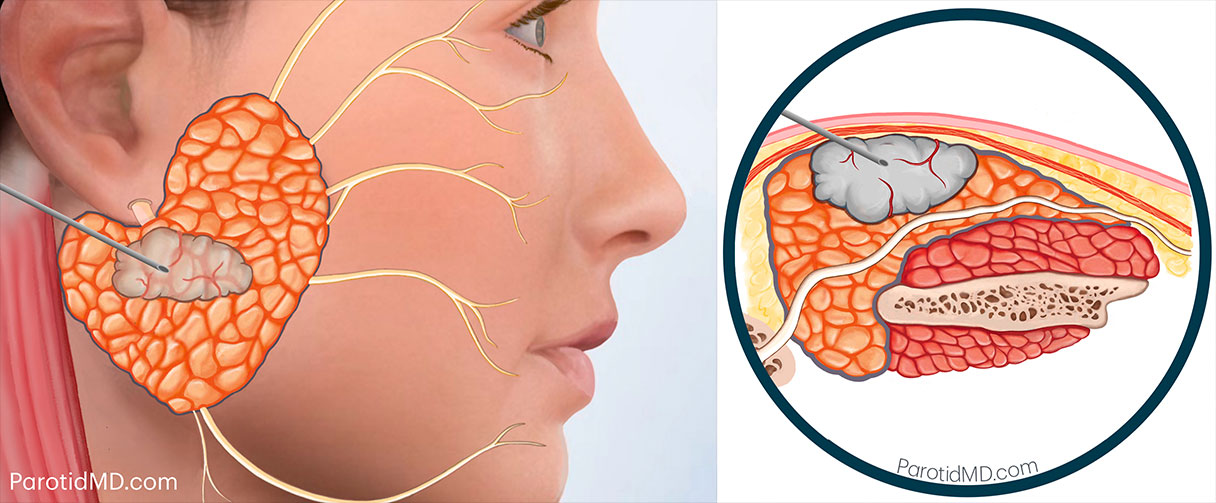
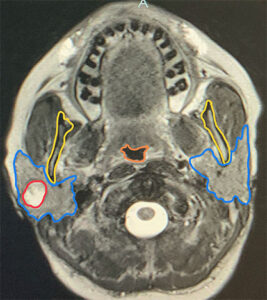
Unfortunately not. The facial nerve is not visible on any scans, so when on a scan a tumor is seen in the parotid gland, it is impossible to tell if there is a nerve adjacent or inside the tumor.
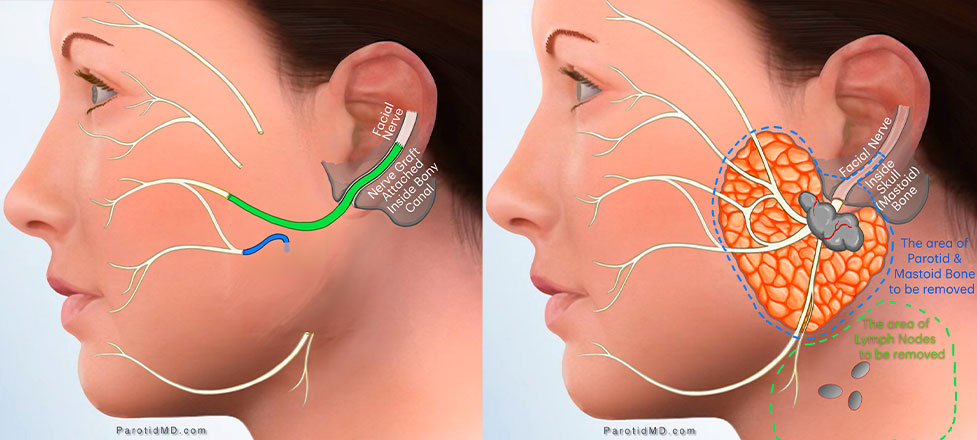
The bony canal of the facial nerve in the skull is visible on CT scan, so if the cancer has invaded the skull bone (mastoid bone), then it can be seen to be in the canal.
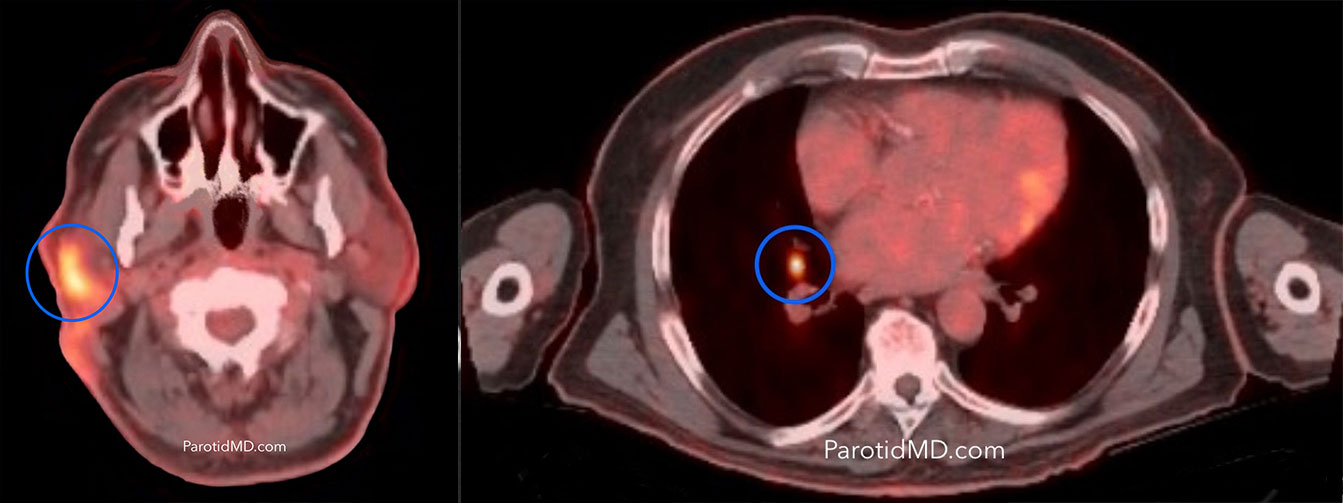
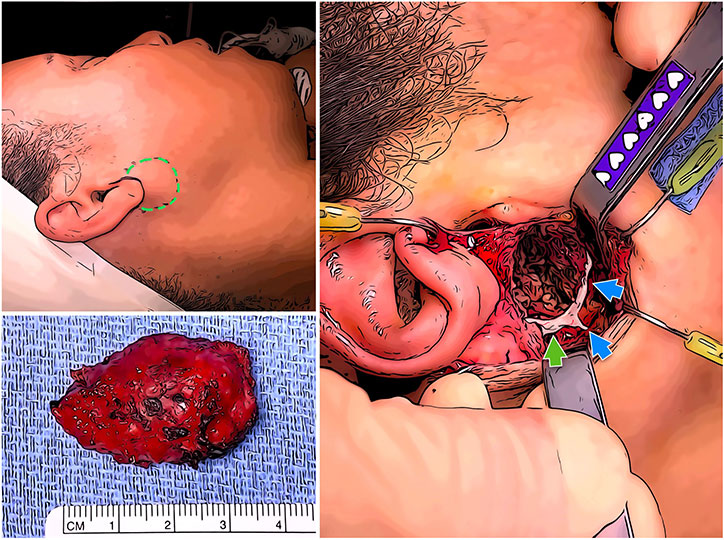
Do other cancers besides skin cancers spread to the parotid gland?
Although rare, some types of cancers can spread from other parts of the body (organs) to the parotid gland. For example, renal cell cancers (kidney cancers) on occasion can spread to the parotid. Usually, a needle biopsy can tell us what type of cancer and potentially where it originated from. If a needle biopsy fails to pinpoint the cancer’s origin, we use a PET scan, which comprehensively scans the entire body.
Are there cancers that have a higher af finity for the facial nerve?
Yes. Some types of cancers, speci fically adenoid cystic carcinoma, like invading the nerve and traveling on then nerve or eating through it. When we encounter these types of cancers our degree of suspicion for nerve involvement is raised and speci fically look for it
Can parotid cancers invade the skull?
Unfortunately yes. There are two mechanisms to get into the skull. 1) Once the cancer has grown large enough to touch the skull (mastoid bone) then it can directly eat through the bone and grow into it. 2) The facial nerve leaves the brain and goes through a long bony canal to exist the skull and immediately enter the parotid gland before dividing into multiple branches. A parotid cancer that has migrated onto the facial nerve can travel up the nerve to enter the skull; it can potentially travel all the way up to the brain.